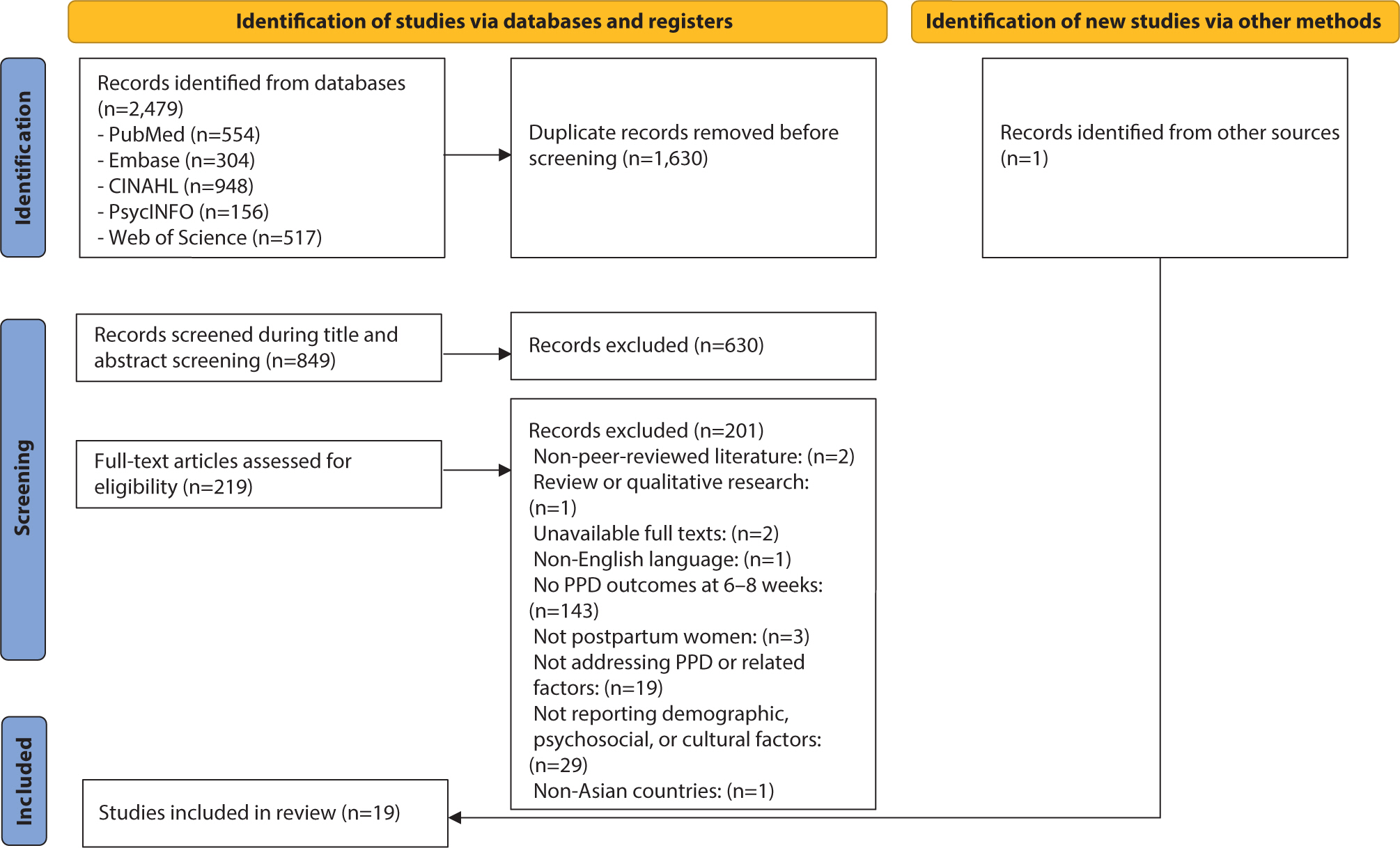
The prevalence of postpartum depression (PPD) in Asia is reported to range from 13.53% to 22.31%. However, there remains a gap in the identification of PPD, particularly regarding cultural cutoff points. Therefore, the purpose of this scoping review was to determine the prevalence and associated factors of PPD in Eastern, South-eastern, Western, and Southern Asian countries and analyze the cutoff points of the Edinburgh Postnatal Depression Scale (EPDS) used across these countries. Following Arksey and O'Malley’s five-step scoping review framework, the population was defined as mothers, the concept as the EPDS, and the context as the Asian region. A literature search was conducted using PubMed, Embase, CINAHL, PsycINFO, and Web of Science. The data analysis focused on demographic characteristics, EPDS cutoffs and features, PPD prevalence, and its associated factors. Nineteen studies were selected. Most countries used translated versions of the EPDS with demonstrated reliability and validity. The cutoff scores varied, with most using scores of 10 or higher. The prevalence of PPD ranged from 5.1% to 78.7%. Key associated factors for PPD included cultural factors such as relationships with in-laws and preferences for the newborn’s sex. To improve the accuracy of PPD screening in Asia, the EPDS should be used consistently, and appropriate cutoff criteria must be established. In addition, prevention strategies and programs that reflect the cultural characteristics and social context of Asia need to be developed for the early detection and prevention of PPD.
Citations

 , Jieun Jang
, Jieun Jang , Nayoung Kim
, Nayoung Kim
Citations

 , Eunha Kim
, Eunha Kim
Neurodevelopmental disorders, which emerge early in development, include a range of neurological phenotypes and exhibit marked differences in prevalence between sexes. A male predominance is particularly pronounced in autism spectrum disorder (ASD). Although the precise cause of ASD is still unknown, certain genetic variations and environmental influences have been implicated as risk factors. Preclinical ASD models have been instrumental in shedding light on the mechanisms behind the sexual dimorphism observed in this disorder. In this review, we explore the potential processes contributing to sex bias by examining both intrinsic differences in neuronal mechanisms and the influence of external factors. We organize these mechanisms into six categories: 1) sexually dimorphic phenotypes in mice with mutations in ASD-associated genes related to synaptic dysfunction; 2) sex-specific microglial activity, which may disrupt neural circuit development by excessively pruning synapses during critical periods; 3) sex steroid hormones, such as testosterone and allopregnanolone, that differentially influence brain structure and function; 4) escape from X chromosome inactivation of the O-linked-N-acetylglucosamine transferase gene in the placenta; 5) sexually dimorphic activation of the integrated stress response pathway following maternal immune activation; and 6) immunological responses that are differentially regulated by sex. Understanding these mechanisms is essential for deciphering the underlying causes of ASD and may offer insights into other disorders with notable sex disparities.
Citations

 , Won Kim
, Won Kim
Understanding the effects of sex and sex differences on liver health and disease is crucial for individualized healthcare and informed decision-making for patients with liver disease. The impact of sex on liver disease varies according to its etiology. Women have a lower prevalence of metabolic dysfunction-associated steatotic liver disease (MASLD) than men. However, postmenopausal women face a higher risk of advanced liver fibrosis due to hormonal influences. Sex differences affect the pathogenesis of MASLD, which involves a complex process involving several factors such as hormones, obesity, and the gut microbiome. Furthermore, sex-related differences in the development of MASLDrelated hepatocellular carcinoma have been observed. The sex-specific characteristics of MASLD necessitate an individualized management approach based on scientific evidence. However, research in this area has been lacking. This article reviews the current understanding of sex differences in MASLD.
Citations

 , Heisook Lee
, Heisook Lee
This review aims to highlight the importance of research on structural, functional, molecular-biological, and disease-specific sex differences in the brain, and to examine current bibliometric indicators related to research on sex differences. The Web of Science Core Collection was searched for related articles from 2010 to 2023. Structural and functional brain differences according to sex, including variations in communication patterns between hemispheres, may play a role in mental disorders. Sex differences in neurotransmitters such as serotonin, dopamine, and γ-aminobutyric acid contribute to disparities in mental health, addiction, and neurodevelopmental conditions. Neurodevelopmental disorders such as autism spectrum disorder and schizophrenia exhibit sex-based differences in prevalence, symptoms, brain changes, and neurotransmitter disruptions under hormonal influence. There is a growing body of research on depression, adolescence, the hippocampus, the amygdala, and cognition, highlighting the importance of considering sex/gender factors. Recent studies on sex differences in brain diseases have identified variations in brain structure, function, and neurophysiological substances, as well as in hormones and genes between the sexes. The incidence of psychiatric disorders such as autism spectrum disorder, depression, anxiety, and Alzheimer’s disease is increasingly being linked to sex differences, and the need for research into the mechanisms underlying these differences is gaining recognition. However, there remains a significant gap in sex-specific neuroscience research related to the diagnosis, treatment, prevention, and management of these conditions. Advancing inclusive research will require comprehensive training, a consensus on methodology, diverse perspectives through collaborative frameworks, governmental/institutional support, and dedicated funding to create suitable research environments and implementation strategies.
Citations


Heart failure (HF) represents a serious public health concern, characterized by substantial morbidity and mortality. Despite advances in pharmacological management, a gap persists in understanding and accounting for sex-related differences in HF treatment. This review was performed to clarify the impact of sex on the clinical outcomes of HF medications. Insights from various clinical trials and studies have highlighted differences between men and women in drug responses and adverse effects, indicating the need for a more nuanced approach to HF management. Promoting greater representation of women in clinical trials and the development of research methodologies that consider sex differences are crucial steps in advancing precision medicine. Such efforts ensure that therapeutic strategies are optimally tailored to the unique biological and genetic profiles of each person. Ultimately, this review emphasizes the vital need for a more inclusive and personalized approach to HF pharmacotherapy, underscoring the critical role of sex-related differences in shaping effective and individualized treatment pathways.
Citations

 , Jong Kil Nam
, Jong Kil Nam , Bon Jin Koo
, Bon Jin Koo , Hyun Jung Lee
, Hyun Jung Lee , Tae Un Kim
, Tae Un Kim , Hwaseong Ryu
, Hwaseong Ryu , Yun Jeong Hong
, Yun Jeong Hong , Seungsoo Lee
, Seungsoo Lee , Dong Hoon Lee
, Dong Hoon Lee , Sung Woo Park
, Sung Woo Park
The aim of this study was to examine the clinical presentation, treatment delivery, and cisplatin eligibility of Korean patients with urothelial carcinoma (UC) in a real-world setting.
We performed a retrospective cohort study of patients initially diagnosed with UC from March 2013 to June 2018. Creatinine clearance >60 mL/min and Eastern Cooperative Oncology Group performance status (0-1) were adopted as cisplatin eligibility criteria.
This study included 557 eligible patients. Median age was 71.0 years (range, 33-94 years), and males were dominant (80%). Primary tumor sites were: upper genitourinary tract, 18%; bladder, 81%; and urethra, 0.4%. Initial disease status was non-muscle invasive bladder cancer (313, 56%), diffuse infiltrating non-muscle invasive bladder cancer (19, 3%), cTanyN0 upper tract UC (75, 13%), cT2-4N0 bladder UC (82, 15%), TanyN1-3 UC (36, 7%), or initially metastatic UC (32, 6%). At the time of analysis (June 2019), following treatments were delivered to 134 patients with localized UC: radical operation with or without perioperative treatment (89, 67%), definitive chemoradiation (7, 5%), and palliative surgery or supportive care only (36, 28%). In total, 89 patients had metastatic UC, including those with recurrent disease (n=57), and 34 (38%) of the 89 were eligible for cisplatin.
Clinical presentations in East Asian UC patients were consistent with those of previous studies in other countries, except for a relatively high incidence of upper genitourinary tract. Our results can serve as a benchmark for further advances and future research for treatments of UC in East Asian patients.
Citations

 , Honkeun Cho
, Honkeun Cho , Si-Hoon Park
, Si-Hoon Park , Gil Ja Shin
, Gil Ja Shin , Dong Su Lee
, Dong Su Lee , Yang Hee Lim
, Yang Hee Lim
The Measurement of blood pressure by a doctor may trigger a pressor response, so there are marked differences between office and ambulatory or self-measured blood pressure and the subjects may misdiagnosed as hypertensives and receive unneccesary medication. The study is designed to evaluate the charicteristic of white coat hypertension, the degree of white coat effect and the relationship between the white coat hypertension and persistent hypertension.
Thirteen patients with office hypertension receiving no medication, were recruited from 434 patients experienced in ambulatory blood pressure. Past history, physical examination, office blood pressure, 12-channel standard electrocardiography, chest X-ray, plasma lipid battery, echocardiography and 24-hr ambulatory blood pressure monitoring with BP3 MEDIANA were performed.
1) White coat hypertensive patients were 13 of 434 patients(2.99%) who were performed 24-hr ambulatory blood pressure monitoring. The mean age was 45±12 years with 6 men and 7 women and rage of age was 26-65 years.
2) The lipid battery, chest X-ray and 12-channel standard electrocardiographty showed no significant finding.
3) The LV mass index was 90.7±11.0g/m3 but one of 8 who performed echocardiography showed concentric hypertrophty.
4) The LV ejection traction was 60.8±8.7% which normal range.
5) The mitral flow velocity parameters were E velocity 0.71±0.14m/sec, A velocity 0.54±0.24m/sec, E/A ratio 1.6±0.8, mitral valve deceleration time 214±27.6msec and isovolumic relaxation time 104±11.4msec but one of 8 showed LV relaxation abnormality.
6) The mean office systolic blood pressure was 159±13.8mmHg, mean office diastolic blood pressure 101±9.0mmHg, 24-hr mean ambulatory systolic blood pressure 128±4.9mmHg and 24-hr diastolic bliid pressure 82±8.6mmHg.
7) The night day ratio of systolic blood pressure was 0.93±0.06 and the night day ratio of diastolic blood pressure was 0.92±0.06 suggestive of blunted diurnal variation. The Dipper were 5 of 13 patients(38.5%) and the non-Dipper were 8 of 13 patients(61.5%).
8) Two of 13 white coat hypertensives were diagnosed as persistent hypertensives in follow-up periods and antihypertensive drug had been initiated.
White coat hypertension can be diagnosed by 24-hr ambulatory blood pressure monitoring. The influence of white coat effect to cardiovascular system was not established. Sixty-two percent of white coat hypertensives showed blunted diurnal variation in 24-hr ambulatory blood pressure monitoring and two of 13 were diagnosed as persistent hypertensives in our F/U study, so white coat effect cannot be merely innocent and need strict evaluation and regular follow-up.
 , Gi Beom Hwang
, Gi Beom Hwang , Hye Jean Lee
, Hye Jean Lee
The purpose of this study is investigating variables affecting the numbers of clinical laboratory tests.
Data about the number of clinical laboratory tests, hospital characteristics, and the number of patients between January 1999 and December 1999 was collected. Data resources were Statistical Yearbook, Standardization Audit by Korean Hospital Association and Internal Data Set of each hospital. Hospital characteristics were hospital ownership, tertiary care hospital, duration since opening, licensed hospital beds, the rates of medical inpatient and outpatient. Multiple regression analysis was applied to find factors affecting the number of clinical laboratory tests. Models for WBC, RBC, Hb, Hct, PLT, LDC, PT, PTT, AST, ALT, and GLU were statistically adequate.
As the results, hospital ownership, duration since opening, licensed hospital beds, the rate of medical outpatient were statistically significant. Private hospitals showed higher numbers than public hospitals, hospitals within 5 years since opening showed higher numbers than others. The licensed hospital beds was positively correlated with the numbers of the tests, whereas the rates of medical outpatient was negatively correlated.
In conclusion, hospital characteristics affect the numbers of clinical laboratory tests. It could be a clue why the costs of medical services were different among medical facilities.

