 , Jooyoung Choi
, Jooyoung Choi
 , Bruno B. Andrade
, Bruno B. Andrade , Ju Sang Kim
, Ju Sang Kim , Yoolwon Jeong
, Yoolwon Jeong
Citations

 , Taek Chung
, Taek Chung , Dong Kyu Kim
, Dong Kyu Kim , Hyungjin Rhee
, Hyungjin Rhee
Intrahepatic cholangiocarcinoma (iCCA) is a heterogeneous bile duct adenocarcinoma with a rising global incidence and a poor prognosis. This review aims to present a comprehensive overview of the most recent radiological research on iCCA, focusing on its histopathologic subclassification and the use of imaging findings to predict prognosis and inform treatment decisions. Histologically, iCCA is subclassified into small duct (SD-iCCA) and large duct (LD-iCCA) types. SD-iCCA typically arises in the peripheral small bile ducts and is often associated with chronic hepatitis or cirrhosis. It presents as a mass-forming lesion with a relatively favorable prognosis. LD-iCCA originates near the hepatic hilum, is linked to chronic bile duct diseases, and exhibits more aggressive behavior and poorer outcomes. Imaging is essential for differentiating these subtypes and assessing prognostic factors like tumor size, multiplicity, vascular invasion, lymph node metastasis, enhancement patterns, and intratumoral fibrosis. Imaging-based prognostic models have demonstrated predictive accuracy comparable to traditional pathological staging systems. Furthermore, imaging findings are instrumental in guiding treatment decisions, including those regarding surgical planning, lymphadenectomy, neoadjuvant therapy, and the selection of targeted therapies based on molecular profiling. Advancements in radiological research have improved our understanding of iCCA heterogeneity, facilitating prognosis prediction and treatment personalization. Imaging findings assist in subclassifying iCCA, predicting outcomes, and informing treatment decisions, thus optimizing patient management. Incorporating imaging-based approaches into clinical practice is crucial for advancing personalized medicine in the treatment of iCCA. However, further high-level evidence from international multicenter prospective studies is required to validate these findings and increase their clinical applicability.
 , YoungMoon Goh
, YoungMoon Goh , Jungwon Kwak
, Jungwon Kwak
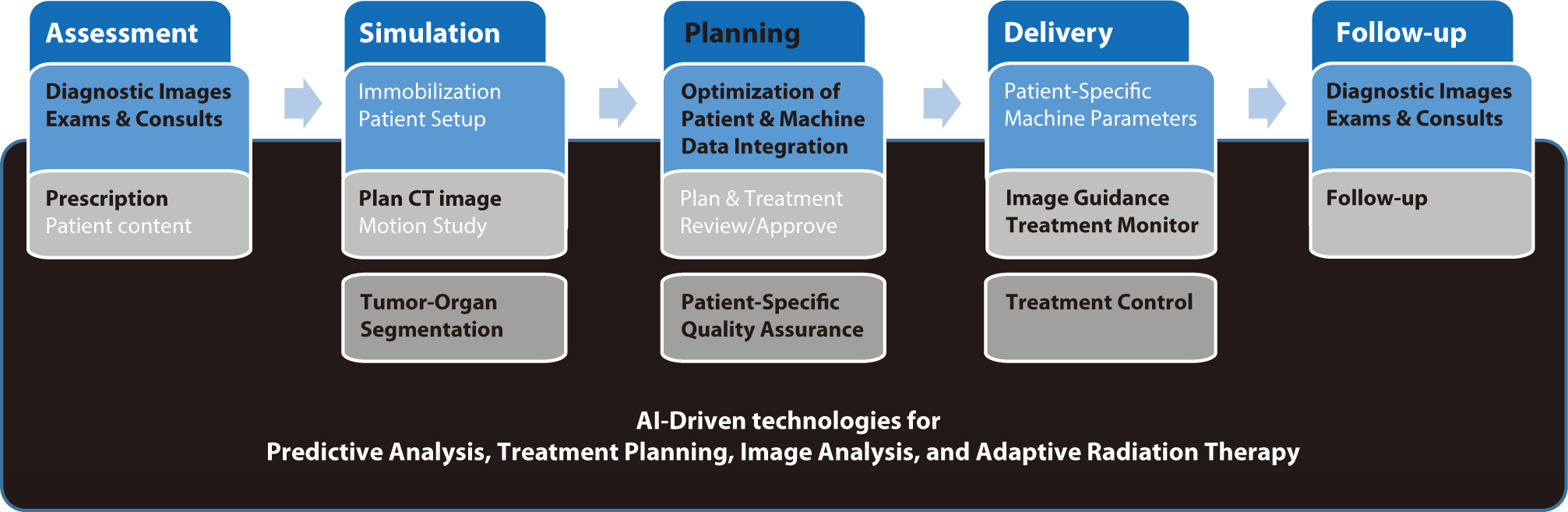
Artificial intelligence (AI) is rapidly transforming various medical fields, including radiation oncology. This review explores the integration of AI into radiation oncology, highlighting both challenges and opportunities. AI can improve the precision, efficiency, and outcomes of radiation therapy by optimizing treatment planning, enhancing image analysis, facilitating adaptive radiation therapy, and enabling predictive analytics. Through the analysis of large datasets to identify optimal treatment parameters, AI can automate complex tasks, reduce planning time, and improve accuracy. In image analysis, AI-driven techniques enhance tumor detection and segmentation by processing data from CT, MRI, and PET scans to enable precise tumor delineation. In adaptive radiation therapy, AI is beneficial because it allows real-time adjustments to treatment plans based on changes in patient anatomy and tumor size, thereby improving treatment accuracy and effectiveness. Predictive analytics using historical patient data can predict treatment outcomes and potential complications, guiding clinical decision-making and enabling more personalized treatment strategies. Challenges to AI adoption in radiation oncology include ensuring data quality and quantity, achieving interoperability and standardization, addressing regulatory and ethical considerations, and overcoming resistance to clinical implementation. Collaboration among researchers, clinicians, data scientists, and industry stakeholders is crucial to overcoming these obstacles. By addressing these challenges, AI can drive advancements in radiation therapy, improving patient care and operational efficiencies. This review presents an overview of the current state of AI integration in radiation oncology and insights into future directions for research and clinical practice.
Citations


The rate of colorectal cancer (CRC) has altered. Early-onset CRC patients are increasing, and it is one of the main causes of cancer-related death. Based on epidemiologic change, the CRC screening program needs to be changed. To increase compliance, non-invasive screening techniques are developed. Although CRC survival has increased, the oncologic prognosis of metastatic CRC is remains poor. Even in metastatic CRC, which is the most difficult to treat, attempts are being made to increase the survival rate by active surgical therapy with the creation of chemotherapeutic regimens and targeted treatment based on genomic information. Due to the introduction of aggressive chemotherapy regimens, targeted therapy based on genomic features, and improvements in surgical technique, the role of surgical treatment in metastatic CRC has expanded. Metastatic CRC surgery was indicated for liver, lung, and even peritoneal seeding. Local ablation therapy was also effectively used for liver and lung metastasis. Cytoreductive surgery and intraperitoneal chemotherapy were tried for peritoneal seeding and demonstrated good results in a subgroup of patients, although the right indication was carefully assessed. At the same time, one of the key goals of treatment for CRC was to maintain functional outcomes. Neoadjuvant treatment, in particular, helped rectal cancer patients preserve functional results while maintaining oncologic safety. Rectal cancer organ preservation techniques are now being researched heavily in a variety of neoadjuvant treatment settings, including immunotherapy and whole neoadjuvant therapy. Precision medicine based on patient and disease characteristics is currently being used for the diagnosis and treatment of CRC.
Citations


