Abstract
Patients with congenital insensitivity to pain and anhidrosis (CIPA) exhibit an inability to perceive pain, recurrent fractures, self-mutilation, and impaired thermoregulation, which lead to severe complications and high morbidity. Children with CIPA often sustain multiple unnoticed fractures that may be mistaken for child abuse because of the presence of fractures at different stages of healing. If unrecognized or inadequately managed, these injuries can cause permanent damage. We report the case of a 9-year-old boy who presented with recurrent fractures, chronic osteomyelitis, heterotrophic ossification, and gangrene. This case underscores the need for heightened awareness among healthcare providers regarding the clinical manifestations and management challenges of CIPA. It also emphasizes the importance of early diagnosis, meticulous follow-up, and a multidisciplinary approach to optimize outcomes and prevent severe complications in affected children.
-
Keywords: Child; Congenital pain insensitivity; Hypohidrosis; Multiple fractures; Osteogenesis; Case reports
Introduction
Background
Congenital insensitivity to pain with anhidrosis (CIPA), classified as hereditary sensory and autonomic neuropathy type IV, is a rare autosomal recessive disorder [
1]. Clinically, patients with CIPA present with a distinct spectrum of symptoms, including congenital insensitivity to pain, anhidrosis, frequent injuries, and varying degrees of autonomic dysfunction [
2].
The inability to perceive pain predisposes patients to repeated trauma, fractures, and self-inflicted injuries, often resulting in severe orthopedic complications such as malunion and chronic osteomyelitis [
3].
Orthopedic complications in CIPA are a major cause of morbidity. Recurrent fractures, joint deformities, and heterotrophic ossification (HO) frequently require surgical intervention and long-term management [
4]. Chronic infections such as osteomyelitis are also common, arising from trauma-related open wounds, poor healing, and impaired immune responses. These infections are often resistant to standard therapies and necessitate a multidisciplinary management approach [
5]. The rarity of CIPA presents considerable challenges in developing evidence-based treatment protocols [
6].
We report a child with recurrent fractures originating from CIPA in Saudi Arabia to raise awareness of differentiating such cases from child abuse.
Case presentation
Ethics statement
Ethical approval was obtained from the Research Ethics Committee of the Makkah Region Health–Ministry of Health (20/05/2025, IRB: H-02-K-076-0425-1340). The patient’s parents provided written informed consent for the publication of this case and the accompanying images.
Patient information/clinical findings
A 9-year-old boy presented to the emergency department with a chief complaint of painless limping. Radiographic evaluation revealed a non-displaced fracture of the right distal tibia. Conservative management was initiated with an above-knee back slab, analgesia, and close follow-up. Within 3 months, the patient developed swelling in the left leg, and imaging revealed a new painless fracture of the left distal tibia with malunion of the proximal tibia, requiring immobilization with a full above-knee cast.
Diagnostic assessment
A pediatrician was consulted and referred the patient for genetic testing, which confirmed mutations in the NTRK1 gene, establishing the diagnosis of CIPA.
Therapeutic intervention
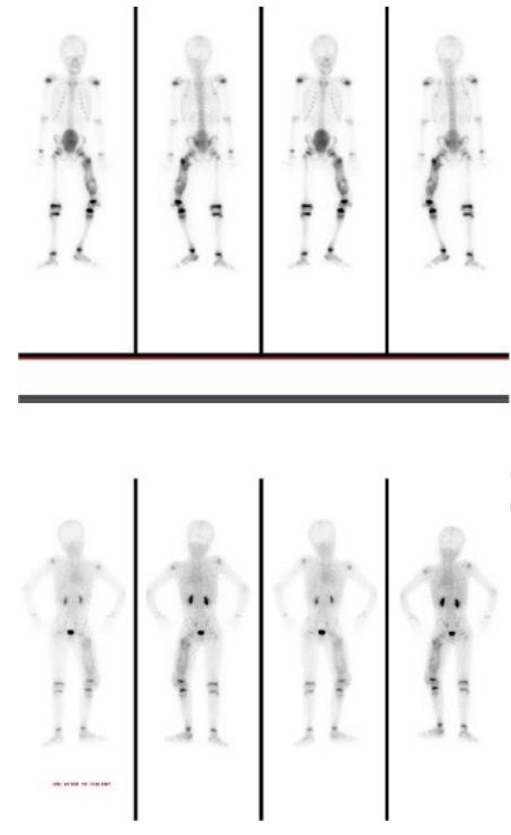
After 5 months, the patient sustained a left femur fracture and was initially stabilized with a temporary back slab, later undergoing surgical intervention with elastic nailing. Persistent concerns regarding abnormal bone healing and possible infection prompted advanced imaging 3 months postoperatively. A Tc99m bone scan revealed active lesions in the femur and tibia (
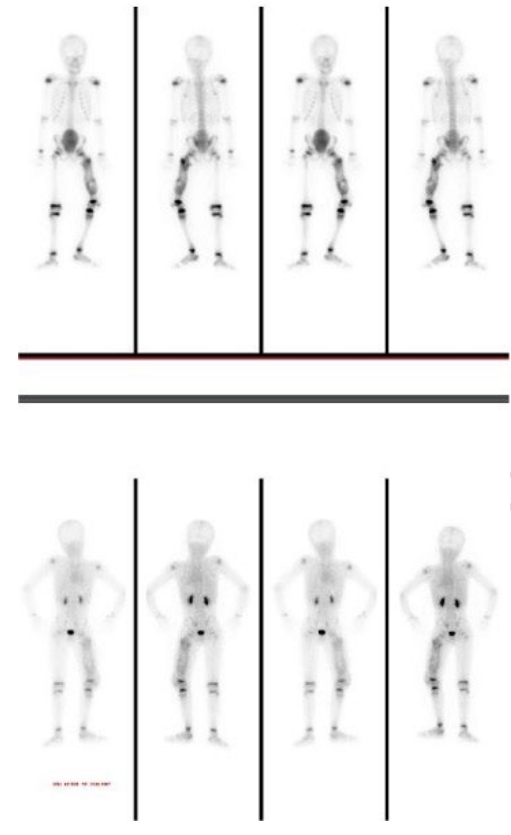
Fig. 1). Computed tomography confirmed chronic osteomyelitis (
Fig. 2) and demonstrated extensive HO. Subsequent management included joint aspirations and scheduled procedures, such as nail removal and bone biopsy.
During follow-up, the patient developed additional complications. He was referred to the plastic surgery team and eventually underwent amputation of the right index finger due to gangrene following necrosis (
Fig. 3).
Discussion
Fractures in patients with CIPA often present atypically because of the absence of pain, and they may go unnoticed until secondary complications such as deformity or swelling occur. Because child abuse is far more prevalent than CIPA, it is crucial to raise awareness among healthcare providers to differentiate CIPA from abuse when evaluating children with recurrent or unexplained fractures [
6].
Our case highlights the multifaceted clinical challenges associated with managing CIPA, including recurrent fractures, chronic infections, and the psychosocial burden of the condition. The patient experienced repeated fractures involving the tibia and femur, frequently accompanied by delayed healing and malunion. Immobilization using above-knee casts remains a cornerstone of fracture management, although surgical interventions such as elastic nailing may be necessary in cases of instability or delayed union [
7,
8].
HO, a rare but recognized complication of CIPA, is characterized by abnormal bone formation in soft tissues, which likely contributed to joint stiffness and impaired mobility in our patient [
9].
Chronic osteomyelitis poses a major concern in CIPA due to recurrent fractures, impaired wound healing, and the absence of pain as a protective mechanism. In this case, repeated infections required bone biopsies, surgical debridement, and, in severe situations, amputation to control disease progression. Multidisciplinary collaboration, including infectious disease specialists, is essential for achieving optimal outcomes. Psychological support and behavioral therapy, supplemented by pharmacological management such as risperidone, are also crucial for addressing behavioral and psychosocial challenges [
10].
These challenges emphasize the need for vigilant monitoring, early imaging, and individualized treatment plans to minimize long-term complications. Current management focuses on symptom control and prevention of secondary sequelae, with regular follow-up to ensure early detection of fractures, infections, and joint deformities [
1,
2]. Early diagnosis and coordinated multidisciplinary care are vital for improving quality of life and functional outcomes in affected individuals.
Since multiple fractures and limb deformities are key orthopedic manifestations of CIPA [
11-
14], it is reasonable for concerns to arise regarding child abuse. Nonetheless, we aim to increase awareness among orthopedic surgeons and healthcare professionals regarding children with recurrent fractures arising from CIPA.
-
Authors’ contribution
Conceptualization, methodology, and design of the case report and management of the patient: AMA. Project administration and the important intellectual content: AAA. Manuscript editing, critical revision, and approval of the final version: HAB, KMA. Patient management, imaging interpretation, and follow-up of the case: RMS. Funding acquisition: none. Writing–original draft: AAA. Writing–review & editing: AMA, AAA, HAB, RMS, KMA. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work.
-
Conflict of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Data availability
Not applicable.
-
Acknowledgments
The authors appreciate Dr. Myung-Joo Jang for generously sharing her time.
-
Supplementary materials
None.
Fig. 1.Tc99m MDP bone scan (triple-phase bone scan). Written informed consent for the publication of this image was obtained from the patient.
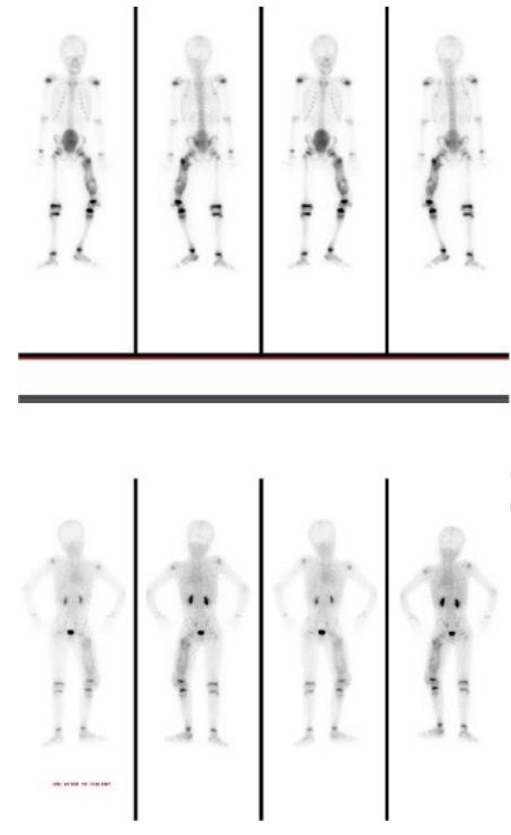
Fig. 2.Noncontrast computed tomography of the left thigh with multiplanar re-formations showing post-nailing fixators in the left femur. Written informed consent for the publication of this image was obtained from the patient.

Fig. 3.Index finger amputation. Written informed consent for the publication of this image was obtained from the patient.

References
- 1. Indo Y. Nerve growth factor and the physiology of pain: lessons from congenital insensitivity to pain with anhidrosis. Clin Genet 2012;82:341-350. https://doi.org/10.1111/j.1399-0004.2012.01943.x
- 2. Indo Y, Tsuruta M, Hayashida Y, Karim MA, Ohta K, Kawano T, Mitsubuchi H, Tonoki H, Awaya Y, Matsuda I. Mutations in the TRKA/NGF receptor gene in patients with congenital insensitivity to pain with anhidrosis. Nat Genet 1996;13:485-488. https://doi.org/10.1038/ng0896-485
- 3. Zhang Y, Haga N. Skeletal complications in congenital insensitivity to pain with anhidrosis: a case series of 14 patients and review of articles published in Japanese. J Orthop Sci 2014;19:827-831. https://doi.org/10.1007/s00776-014-0595-2
- 4. Chalmers J, Gray DB, Rush J. Observations on the induction of bone in soft tissues. J Bone Joint Surg Br 1975;57:36-45. https://doi.org/10.1302/0301-620x.57b1.36
- 5. Ikrama M, Usama M, Haider MH, Israr S, Humayon M. Congenital insensitivity to pain with anhidrosis: a literature review and the advocacy for stem cell therapeutic interventions. Ther Adv Rare Dis 2024;5:26330040241292378. https://doi.org/10.1177/26330040241292378
- 6. Al Amroh HH, Reyes AL, Barret Austin Hillary J, Al Khaffaf WH. Painless: a case of congenital insensitivity to pain in a 5-year-old male. Oxf Med Case Reports 2020;2020:omaa046. https://doi.org/10.1093/omcr/omaa046
- 7. Perez-Lopez LM, Cabrera-Gonzalez M, Gutierrez-de la Iglesia D, Ricart S, Knorr-Gimenez G. Update review and clinical presentation in congenital insensitivity to pain and anhidrosis. Case Rep Pediatr 2015;2015:589852. https://doi.org/10.1155/2015/589852
- 8. Silverman FN, Gilden JJ. Congenital insensitivity to pain: a neurologic syndrome with bizarre skeletal lesions. Radiology 1959;72:176-190. https://doi.org/10.1148/72.2.176
- 9. Gray DH, Speak KS. The control of bone induction in soft tissues. Clin Orthop Relat Res 1979;(143):245-250. https://doi.org/10.1097/00003086-197909000-00039
- 10. Santoya-Montes Y, Gutierrez-Ruiz K, Zequeira Cotes R, Puentes Rozo P. Two case reports of neuropsychological functioning in congenital insensitivity to pain with anhidrosis (CIPA). Dev Neuropsychol 2020;45:414-430. https://doi.org/10.1080/87565641.2020.1825719
- 11. Jarade EF, El-Sheikh HF, Tabbara KF. Indolent corneal ulcers in a patient with congenital insensitivity to pain with anhidrosis: a case report and literature review. Eur J Ophthalmol 2002;12:60-65. https://doi.org/10.1177/112067210201200112
- 12. Algahtani H, Naseer MI, Al-Qahtani M, Abdulrahman SA, Boker F, Shirah B. Congenital insensitivity to pain with anhidrosis: a report of two siblings with a novel mutation in (TrkA) NTRK1 gene in a Saudi family. J Neurol Sci 2016;370:35-38. https://doi.org/10.1016/j.jns.2016.09.016
- 13. Altassan R, Saud HA, Masoodi TA, Dosssari HA, Khalifa O, Al-Zaidan H, Sakati N, Rhabeeni Z, Al-Hassnan Z, Binamer Y, Alhashemi N, Wade W, Al-Zayed Z, Al-Sayed M, Al-Muhaizea MA, Meyer B, Al-Owain M, Wakil SM. Exome sequencing identifies novel NTRK1 mutations in patients with HSAN-IV phenotype. Am J Med Genet A 2017;173:1009-1016. https://doi.org/10.1002/ajmg.a.38120
- 14. Alobaida S, Lam JM. Bilateral harlequin syndrome, unilateral Horner syndrome, and Riga-Fede disease as presenting features of hereditary sensory and autonomic neuropathy type IV. Pediatr Dermatol 2021;38:213-216. https://doi.org/10.1111/pde.14385
Citations
Citations to this article as recorded by