
 , Zekeriya Temircan
, Zekeriya Temircan
The present study aims to examine the frequency of sleep disorders and the level of sleep quality, as well as their relationship with health-related quality of life in cancer patients.
This multi-center cross-sectional survey included 333 cancer patients ranging in age from 16 to 72 years, between June 15, 2017, and August 30, 2018 at the Ankara Oncology Hospital and Erciyes University Kemal Dedeman Oncology Hospital Polyclinic. Data were collected via various surveys conducted through face-to-face interviews, including following measurement tools: Short Form 36 Health Questionnaire, the Pittsburgh Sleep Quality Index, the Epworth Sleepiness, and the Berlin Sleep Questionnaire for obstructive sleep apnea. Face-to-face interviews were carried out with patients who presented for an initial examination or follow-up and were awaiting their appointments.
The most commonly reported sleep disorders were daytime sleepiness (36.9%), sleep respiratory disorders (34.8%), insomnia (29.4%), and parasomnias (28.8%). Good sleepers were found to have significantly higher physical (40.20±10.08 vs. 33.21±8.06; P<0.001) and mental component scores (43.54±8.25 vs. 38.20±7.52; P<0.001) than poor sleepers. Conversely, individuals with insomnia (P<0.01), daytime sleepiness (P<0.001), sleep-respiratory disorders (P<0.05), and bruxism (P<0.001) showed significantly lower scores in both physical and mental components. Additionally, those with restless legs syndrome had a significantly lower physical component score (P<0.001), and those with parasomnias had significantly lower mental component scores.
Cancer patients exhibited moderate average sleep quality scores, with over half of them demonstrating low quality sleep patterns. Sleep disorders significantly impacted their health-related quality of life.
Citations

 , Hye-Kyung Jung
, Hye-Kyung Jung , Joo Hee Hong
, Joo Hee Hong , Hye Sook Park
, Hye Sook Park
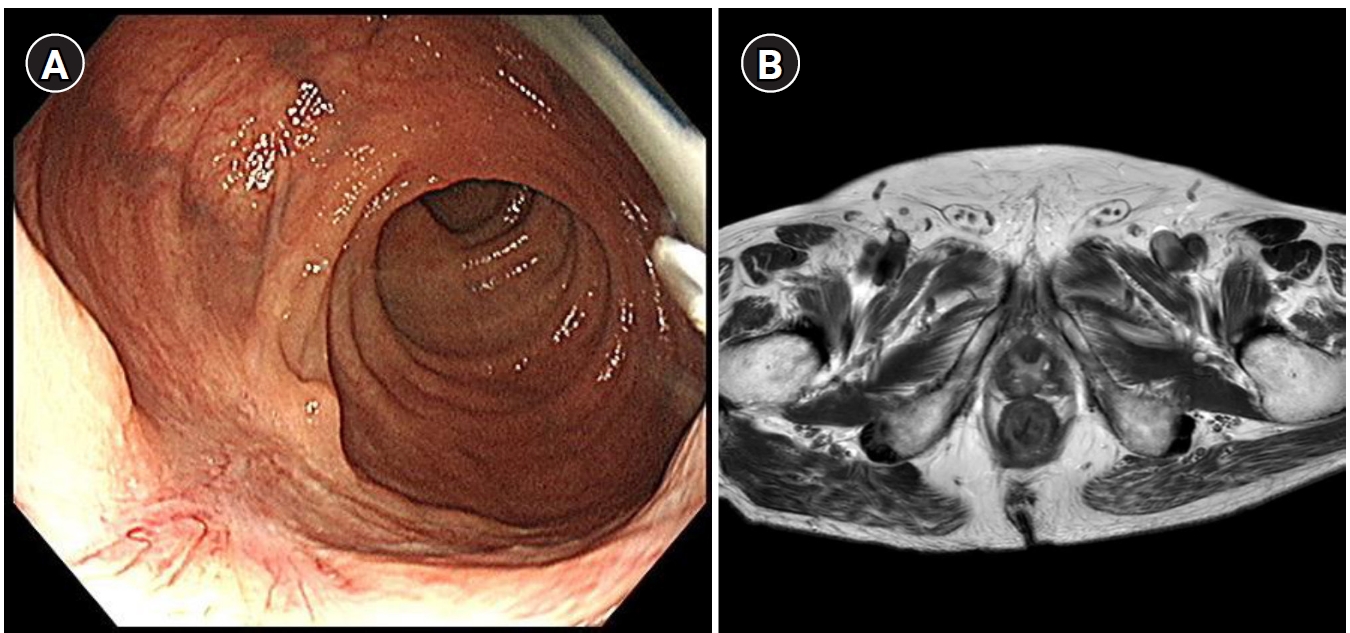
Gastro-esophageal reflux disease(GERD) is increasing in Asian countries, but the majority of patients does not present with endoscopic abnormalities, the assessment of the symptom severity and quality of life, and their response to treatment, have become increasingly important. Our objectives were to develop and evaluate a questionnaire about Health-related quality of lif (HRQOL) related with gastrointestinal symptoms in patients with GERD.
Eighty eight, consecutive patients with GERD and 174 healthy subjects were enrolled in the study. GERD was defined by the presence of reflux symptom that are heartburn and acid reflux with occurring more than once per week with/without endoscopic reflux esophagitis. All subjects were examined with endoscopy and performed self-reported questionnaires that were modified Korean form of gastrointestinal symptom rating scale(KGSRS), newly developed instrument, and KSF-36(Korean version of Medical Outcomes Study Short Form), a conventional one. We compared the score of KGSRS between response group and non-response group after 2-weeks omeprazole trial for evaluation of discriminative validity of KGSRS.
Internal consistency for the KGSRS scales range from 0.58-0.84. The repeatability was confirmed by test-retest results(Pearson's correlation coefficients=0.62-0.80, p<0.01). The KGSRS scale scores were significantly correlated with those of KSF-36. It revealed construct validity. The total score of KGSRS in patients with GERD was significantly lower than control(376.1±51.3 vs. 433.5±42.0, p=0.000). There were significant differences for 4 symptom complex except diarrhea between response group and non-response group.
The KGSRS has good reliability and construct validity and discriminates symptom severity and frequency of patients with GERD.
Citations

 , Jun Yong Kim
, Jun Yong Kim , Kyong Hun Kim
, Kyong Hun Kim , Dong Seok Kim
, Dong Seok Kim , Yong Chan Lee
, Yong Chan Lee , Ha Na Yoon
, Ha Na Yoon , Young Yo Park
, Young Yo Park
We assessed the quality of life in two different types of urinary diversion ; ileal conduit and orthotopic ileal neobladder through well-validated questionnaire in patients with invasive bladder cancer.
From February 1992 to February 2000, we used a questionnaire consisted of questions about occupational activity, travel, sexual activity, relationship with partner, global satisfactions, etc. in ileal conduit group and orthotopic ileal neobladder group. This questionnaire was scored according to distress from 1 point to 4 point(1 point-no problem, 2 point-a little, 3 point-much, 4 point-very much).
Numbers of patients in ileal conduit group and orthotopic neobladder group were 10 and 6, respectively. Mean age and follow-up period in each group was 72+21 years old, 32+31 month in ileal conduit group, and 55+10 years old. 18+12 months in orthotopic neobladder group. Quality of life in each group showed differences in keeping their jobs, having relationships with others, satisfaction rates about the type of diversion which they have, and overall satisfaction rates.
Even through our data is small in number and relatively short-term in follow-up duration, there are meaningful differences in quality of life and its overall satisfaction rate between ileal conduit group and orthetopic neobladder group. We suggest that it is recommendable to consider not only the surgical outcome but also patients' postoperative quality of life when deciding the type of urinary diversion in advanced bladder cancer patients.

