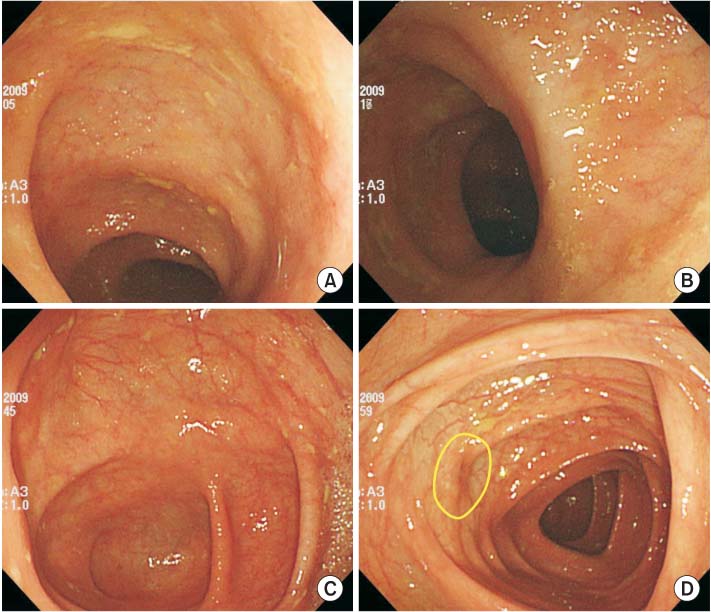
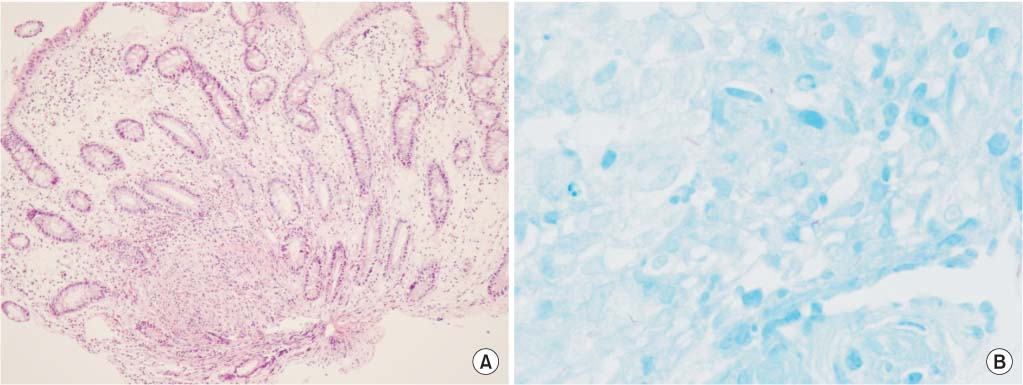
Fig. 1Initial colonoscopic examination. (A, B) Deep and wide ulcerative lesions with irregular margin are observed on the terminal ileum. (C, D) An oval shaped elevated lesion with normal looking mucosa is observed on the ascending colon. The surface mucosal defect is considered as the orifice.
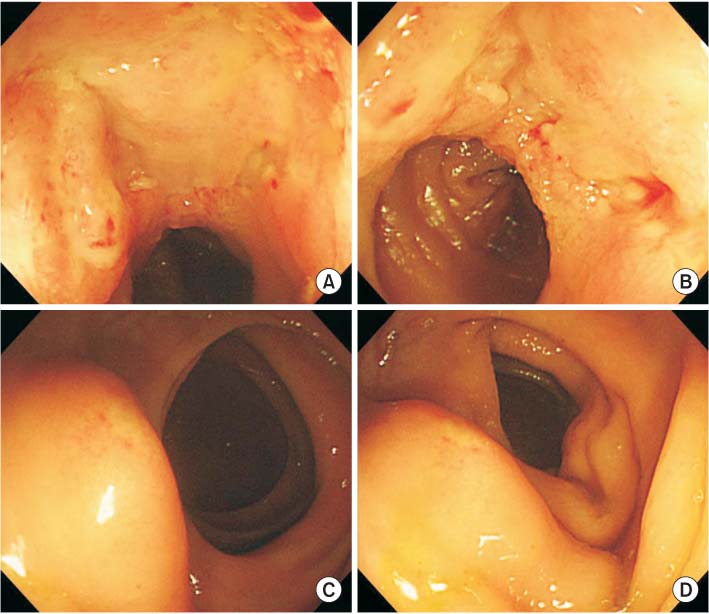
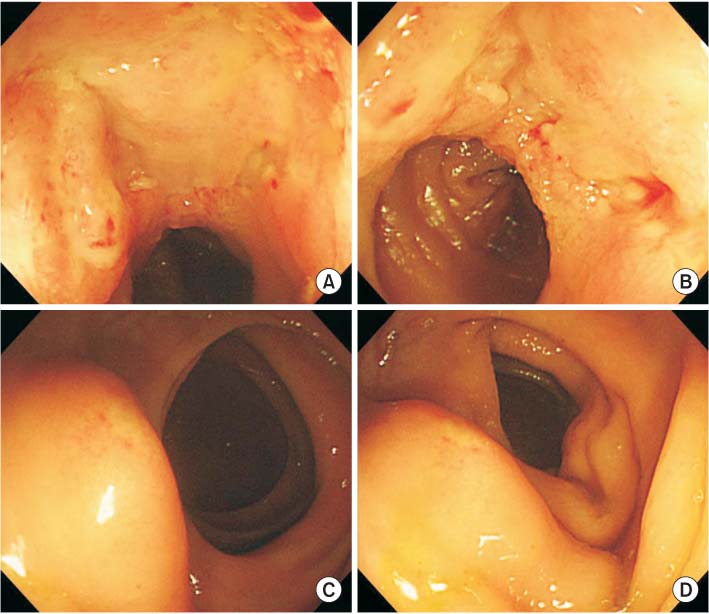
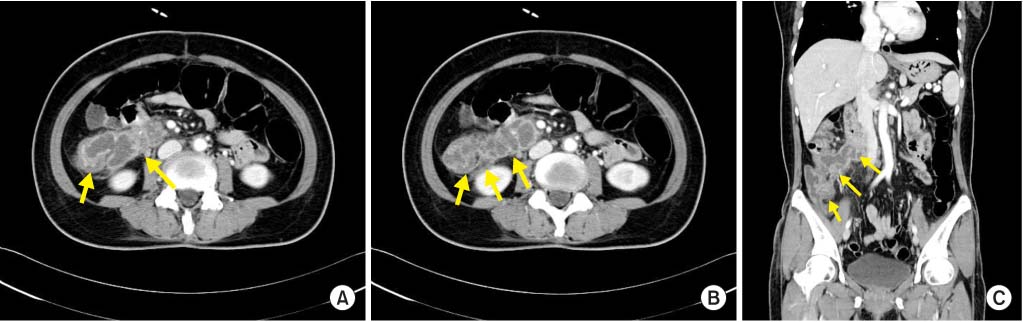
Fig. 2Tissue biopsy findings. (A) Chronic granulomatous inflammation with caseous necrosis is observed (H&E, ×100) (B) AFB are observed on an AFB stain (×400).
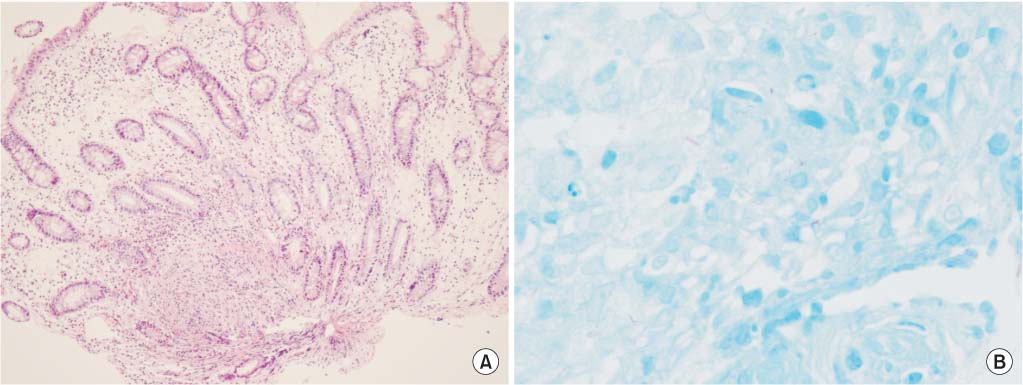
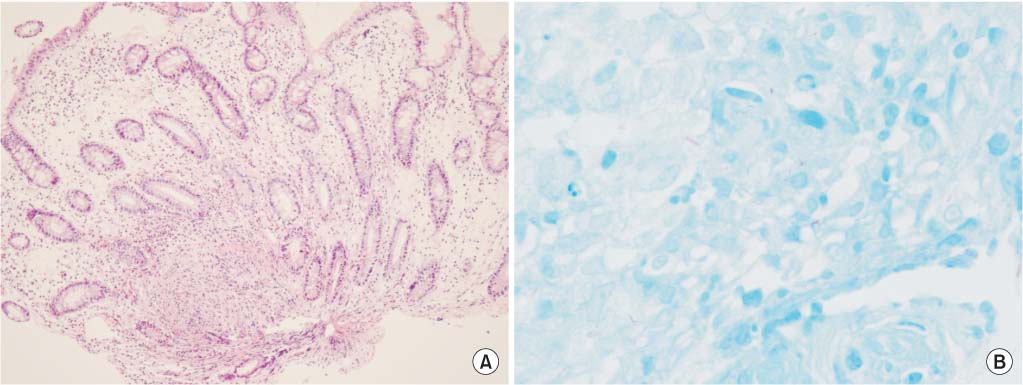
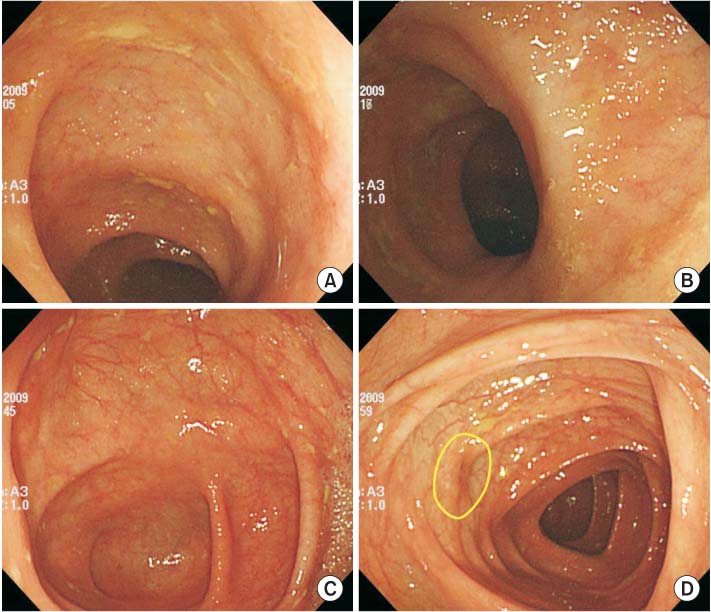
Fig. 3Abdominal computed tomography (CT) findings, sagittal plane (A, B) and transverse plane (C) views. The CT scan shows a thickened terminal ileum, enlargement of multiple lymph nodes and a cold abscess (arrows).
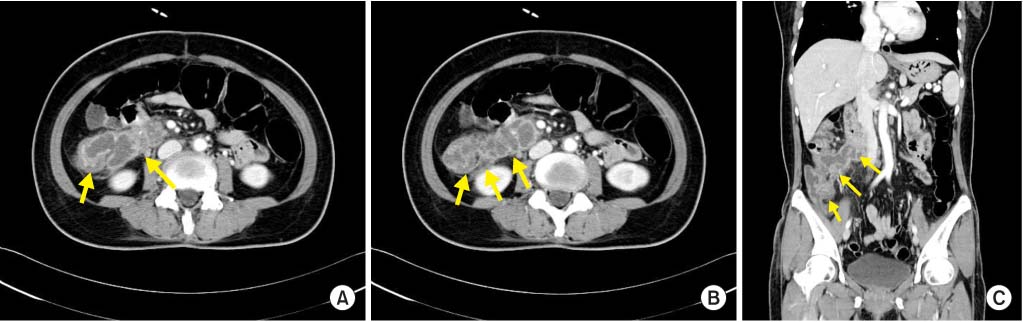
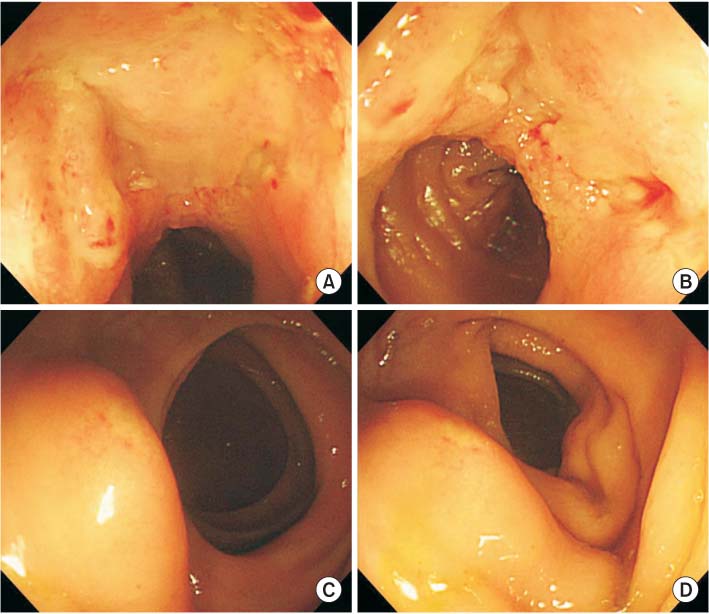
Fig. 4Follow-up colonoscopic examination. (A-C) Ulcerative lesions on the terminal ileum has healed and whitish scars are observed. (D) The orifice and elevated lesion on the ascending colon have disappeared (circle).